top of page
Patient Presentation: A 23-year-old obese female was diagnosed with idiopathic intracranial hypertension (IIH) and referred to neurosurgery for ventriculoperitoneal shunt. A baseline ocular examination was performed prior to the procedure.
On examination, vision was 20/200 in the right eye, and 20/40 in the left eye. There was a right relative afferent pupillary defect. Slit lamp examination was normal.
A dilated fundus examination was performed demonstrating the following:
Ocular Oncology
Case 8
Patient Presentation: A 77-year-old woman presented to an emergency eye clinic with 1-week of right eye floaters. The patient denied trauma, flashes or a curtain over her vision; however, she did note her vision was not as “crisp” in her right eye during this time. She had a significant oncologic history including mucinous adenocarcinoma of the ovary, which was treated with debulking and adjuvant chemotherapy (carboplatin and taxol) 15 years prior and a mastectomy for ductal carcinoma in situ (DCIS) of the left breast 5 years prior. Three months prior to presentation, the patient was found to have metastasis to her adrenal glands, bones and lung. A lung biopsy was performed which found adenocarcinoma with mucinous features. However, there were some differences in immunohistochemistry between ovarian and lung markers. As the origin was presumed ovarian in nature, and the success of prior chemotherapy, the patient was re-started on carboplatin and taxol. Despite multiple cycles of chemotherapy, her metastatic lesions progressed on imaging.
On examination, her visual acuity was 20/30 OD and 20/25 OS. IOP was within normal limits and there was no RAPD. Anterior segment examination was within normal limits. Fundus photographs of the right eye were taken and are shown below:

Question 1: What is the most prominent finding in the fundus photograph above?
Next, B-Scan Ultrasonography and fundus autofluorescence images were taken. The B-Scan below demonstrated a 1.36mm lesion with medium-high internal reflectivity. FAF demonstrated hypo-autofluorescence throughout the lesion seen on fundus imaging.


OCT imaging over the lesion was performed and is shown below:


Question 2: What is the most striking feature of the OCT images above?
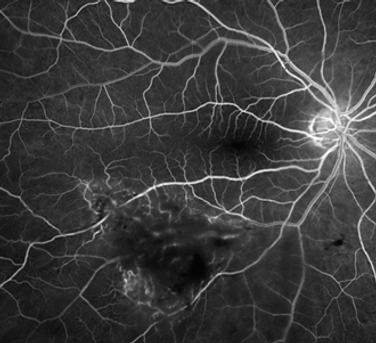
Next, an intravenous fluorescein angiography was performed (shown below) demonstrating retinal vessel telangiectasia and tortuosity with blockage in the early phase, with lake leakage.

Question 3: What is the next best step for this patient’s work-up?
The pathology results of the retinal biopsy are shown below. The histological appearance was consistent with metastatic mucinous adenocarcinoma. Immunohistochemistry was similar to the lung biopsy, which therefore favours a lung primary metastasis over ovarian metastasis.

One month following the change in chemotherapy (from ovarian to lung metastasis), the retinal metastasis regressed, as well as regression of systemic lesions.

Question 4: What should be on your differential for retinal metastasis?
Learning Objectives:
-
Understand the presenting signs and symptoms of retinal metastasis.
-
Learn the use of retinal biopsy and immunohistochemistry in the diagnosis and management of these patients.
-
Understand the typical OCT features of retinal metastasis.
bottom of page
.png)